Health Care Management Report
: Analysis on the Market, Trends, and TechnologiesThe health care management market is accelerating around data-first operations and care models: adoption of digital health platforms rose by 15% over the last two years in the internal health care management data, signaling rapid platform uptake. Market forecasts show sizeable expansion in software and care-management categories — for example, one market projection places the health-care management software market at USD 13.2 billion in 2023 growing to USD 27.9 billion by 2028 (14.9% CAGR), driven by AI analytics, remote monitoring, and value-based payment incentives Global Health Care Management Software Market 2023-2028. These shifts (technology adoption + reimbursement change) create short-term pressure to integrate EHR, telehealth, and analytics while creating medium-term opportunities to capture recurring value from chronic-care, population health, and contract management offerings Population Health Management Market Analysis 2025 Care Management Solutions Market 2025.
We updated this report 142 days ago. Missing information? Contact us to add your insights.
Topic Dominance Index of Health Care Management
The Topic Dominance Index combines the distribution of news articles that mention Health Care Management, the timeline of newly founded companies working within this sector, and the share of voice within the global search data
Key Activities and Applications
- Population health management (PHM): data aggregation, risk stratification and outreach programs used by payers and providers to manage cohorts and measure outcomes Population Health Management Market Analysis 2025.
- Chronic care management (CCM) and remote patient monitoring (RPM): longitudinal monitoring, RPM device ingestion and monthly CCM workflows that generate recurring reimbursements for practices.
- Revenue cycle management (RCM): claims lifecycle automation, denial management and specialty coding to protect provider margins and cash flow.
- Care coordination and transitional care: discharge notifications, care navigator workflows and virtual visit integration to reduce readmissions and improve follow-up rates Manifest MedEx.
- Contract and payer management: CLM and pricing transparency tools for payer/provider negotiations and performance tracking under value-based contracts.
Emergent Trends and Core Insights
- AI moves from pilot to embedded capability. Hospitals and PHM platforms embed predictive risk engines and analytics into workflows to identify high-need patients and measure ROI for value-based contracts Population Health Management Market Analysis 2025.
- Telehealth and RPM permanently shift care pathways. Telehealth integration reduces coordination costs and raises adherence to follow-up (reported provider case studies show material reductions in readmissions when virtual visits are used).
- Value-based care adoption forces operational change: value contracts expanded materially in recent years, increasing demand for platforms that report quality metrics and manage utilization.
- Platform consolidation and specialization run in parallel: buyers favor integrated suites (PHM + CCM + RCM + contract management) but still acquire best-in-class niche modules (e.g. predictive analytics, claims automation) to fill gaps [Company Landscape Report — synthesis integrated across the data].
- Contract management and CLM tools show the fastest software CAGR within administrative segments (projected double-digit growth), driven by compliance and payer negotiation complexity.
Technologies and Methodologies
- Cloud-native PHM and care-management platforms (scalable multi-tenant SaaS for analytics and workflows) Population Health Management Market Analysis 2025.
- Machine learning risk engines and predictive models for readmission risk, utilization forecasting and patient segmentation HBI Solutions, Inc..
- FHIR and API-first interoperability for real-time ADT, claims and device data flow to enable care coordination Population Health Management Market Analysis 2025.
- Telehealth + RPM device integration with automated clinical tasking and escalation rules Care Management Solutions Market 2025.
- Workflow automation and RPA for administrative tasks (eligibility, prior auth, claims scrubbing) and contract metadata extraction (NLP).
Health Care Management Funding
A total of 1.4K Health Care Management companies have received funding.
Overall, Health Care Management companies have raised $68.3B.
Companies within the Health Care Management domain have secured capital from 4.3K funding rounds.
The chart shows the funding trendline of Health Care Management companies over the last 5 years
Health Care Management Companies
- Dulcian Health — Dulcian embeds CCM workflows inside EHRs (athenaClinicals integration) so practices capture Medicare CCM revenue without separate interfaces; the product automates care plan creation, time tracking for CPT billing, and gap-closure reporting to surface revenue opportunities and increase in-house capture Dulcian Health. Dulcian targets small-to-mid practices that want low-friction CCM adoption and keeps revenue within the practice.
- HBI Solutions, Inc. — HBI provides validated predictive analytics and real-time risk modeling that combine clinical, claims and billing data to predict admissions, readmissions and cost events; customers use HBI models to operationalize outreach lists and measure contract risk before taking downside exposure HBI Solutions, Inc.. The firm emphasizes clinically-validated models and ongoing model tuning with provider feedback.
- The Health Co-Lab — The Co-Lab packages a claims+clinical data model and planning tools for community health centers and CBOs to run scenario-based budgeting and staffing benchmarks; it focuses on actionable operational plans that tie to MediCal integration and payer contracting The Health Co-Lab. Their product targets under-resourced health centers that need pragmatic revenue and staffing forecasts.
- HMP Metrics, LLC. — HMP assembles Medicare cost reports and facility financials into a benchmarking and market-analysis dataset used for M&A diligence, strategic planning and peer comparisons; buyers use HMP data to stress-test reimbursement scenarios and evaluate hospital financial health before contracting or acquisition HMP Metrics, LLC.. The dataset supports competitive strategy and rapid target screening.
- MDQ SmartCare — MDQ applies AI to EMR data for coding accuracy, gaps-in-care detection and CCM workflow automation; their technology improves coding consistency and surfaces under-billed chronic care opportunities for practices seeking to monetize care management while improving quality metrics MDQ SmartCare. MDQ focuses on integrating AI into clinician workflows to minimize friction.
(Each company profile above cites the company record and describes how it maps to key activities listed earlier. Company facts and positioning are drawn from the company dataset entries cited.)
Gain a competitive edge with access to 10.4K Health Care Management companies.
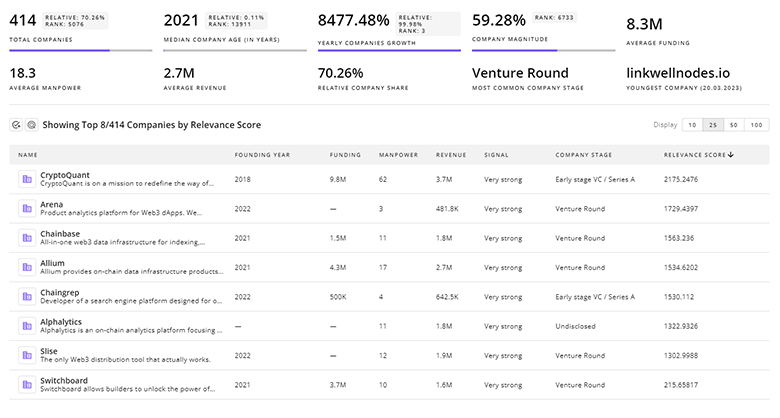
10.4K Health Care Management Companies
Discover Health Care Management Companies, their Funding, Manpower, Revenues, Stages, and much more
Health Care Management Investors
Leverage TrendFeedr’s sophisticated investment intelligence into 3.7K Health Care Management investors. It covers funding rounds, investor activity, and key financial metrics in Health Care Management. investors tool is ideal for business strategists and investment experts as it offers crucial insights needed to seize investment opportunities.
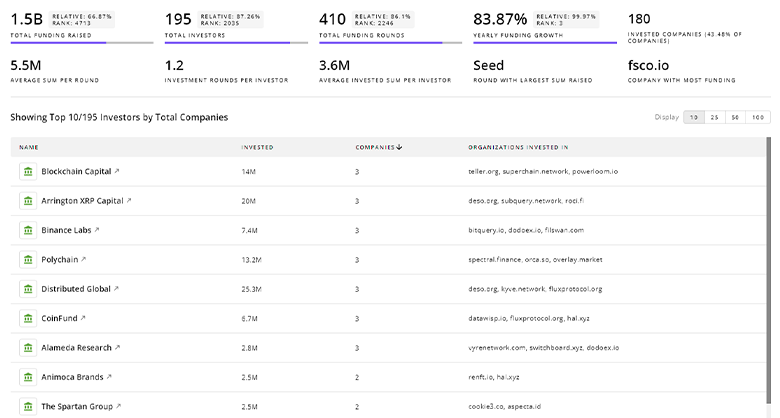
3.7K Health Care Management Investors
Discover Health Care Management Investors, Funding Rounds, Invested Amounts, and Funding Growth
Health Care Management News
TrendFeedr’s News feature provides a historical overview and current momentum of Health Care Management by analyzing 4.4K news articles. This tool allows market analysts and strategists to align with latest market developments.
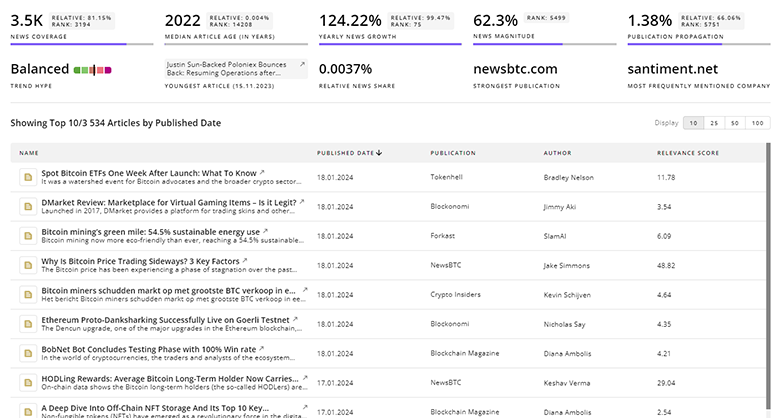
4.4K Health Care Management News Articles
Discover Latest Health Care Management Articles, News Magnitude, Publication Propagation, Yearly Growth, and Strongest Publications
Executive Summary
Health care management is shifting from isolated point solutions to integrated platforms that must prove measurable value under value-based contracts. Short-term priorities for buyers focus on rapid EHR integration, predictable CCM/RPM revenue streams, and claims automation to protect margins. Mid-term winners will combine validated predictive models, seamless interoperability (FHIR/APIs), and modular workflows that let customers deploy targeted capabilities quickly. Niche suppliers with clinically validated analytics or lightweight EHR-embedded CCM tools can capture outsized value by becoming indispensable components of larger platform stacks. For strategic buyers and investors, the most defensible plays are (1) platform expansions that tightly connect clinical outcomes to contract economics, (2) middleware providers that standardize data flows across heterogeneous systems, and (3) services that convert predictive insights into documented contract savings under pay-for-performance arrangements.
Interested in contributing your expertise on trends and tech? We’d love to hear from you.